Connect With Us

Is My Toe Broken?
 There are many signs that can indicate if a person has broken their toe. Common symptoms of a broken toe can include pain when the affected toe is touched, difficulty walking, as well as swelling and bruising. Bruising can appear with vivid discoloration if the injury is extreme. Sometimes the toenail of the affected toe can become severely damaged and show abnormalities if a break has occurred. Blood may become trapped under the toenail causing discoloration. More noticeably, you may see a bone protrude from the affected toe. If you believe you have a broken toe, it’s important that you visit a podiatrist who can provide a proper diagnosis and an advised treatment plan.
There are many signs that can indicate if a person has broken their toe. Common symptoms of a broken toe can include pain when the affected toe is touched, difficulty walking, as well as swelling and bruising. Bruising can appear with vivid discoloration if the injury is extreme. Sometimes the toenail of the affected toe can become severely damaged and show abnormalities if a break has occurred. Blood may become trapped under the toenail causing discoloration. More noticeably, you may see a bone protrude from the affected toe. If you believe you have a broken toe, it’s important that you visit a podiatrist who can provide a proper diagnosis and an advised treatment plan.
Broken toes may cause a lot of pain and should be treated as soon as possible. If you have any concerns about your feet, contact one of our podiatrists from Florida Foot & Ankle Group, P.A.. Our doctors will treat your foot and ankle needs.
What Is a Broken Toe?
A broken toe occurs when one or more of the toe bones of the foot are broken after an injury. Injuries such as stubbing your toe or dropping a heavy object on it may cause a toe fracture.
Symptoms of a Broken Toe
- Swelling
- Pain (with/without wearing shoes)
- Stiffness
- Nail Injury
Although the injured toe should be monitored daily, it is especially important to have a podiatrist look at your toe if you have severe symptoms. Some of these symptoms include worsening or new pain that is not relieved with medication, sores, redness, or open wounds near the toe.
If you have any questions, please feel free to contact one of our offices located in Debary, Lake Mary, Orlando, and Oviedo, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What to Know About a Broken Toe
Trauma to the foot, especially the toes, can occur in many ways. Banging them, stubbing them, or dropping something on them are a few different ways this trauma can occur. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break or fracture. Another type of trauma that can break a toe is repeated activity that places stress on the toe for prolonged periods of time.
Broken toes can be categorized as either minor or severe fractures. Symptoms of minor toe fractures include throbbing pain, swelling, bruising on the skin and toenail, and the inability to move the toe with ease. Severe toe fractures require medical attention and are indicated when the broken toe appears crooked or disfigured, when there is tingling or numbness in the toe, or when there is an open, bleeding wound present on the toe.
Generally, a minor toe break will heal without long-term complications. However, it is important to discontinue activities that put pressure on the toe. It is best to stay off of the injured toe and immediately get a splint or cast to prevent any more additional movement of the toe bones. You can also immobilize your toe by placing a small cotton ball between the injured toe and the toe beside it. Then, tape the two toes together with medical tape. Swelling can be alleviated by placing an ice pack on the broken toe directly as well as elevating your feet above your head.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery, especially when the big toe has been broken. Due to its position and the pressure the big toe endures with daily activity, future complications can occur if it is not properly treated. Pain associated with minor toe fractures can be managed with over-the-counter pain medications. Prescription pain killers may be necessary for severe toe fractures.
The healing time for a broken toe is approximately four to six weeks. In severe cases where the toe becomes infected or requires surgery, healing time can take up to eight weeks or more. While complications associated with a broken toe are immediately apparent, it is important to note that there are rare cases when additional complications, such as osteoarthritis, can develop over time. You should immediately speak with your podiatrist if you think you have broken your toe due to trauma. They will be able to diagnose the injury and recommend the appropriate treatment options.
How Vitamins Can Help Prevent Cracked Heels
 Cracked heels can be unpleasant to look at and may also cause a great deal of foot pain if left untreated. In serious cases, the cracks may turn into fissures, which are deep cracks in the skin that can lead to bleeding. While cracked heels are linked to dryness of the skin, they may also form due to a vitamin deficiency. If you aren’t getting the proper vitamin intake, the skin may become dry, dull, and prematurely age. Vitamin E is particularly beneficial in protecting collagen in your skin, and can be found in foods such as avocados, mangos, and salmon. For more information on what vitamins may help the prevention of cracked heels, please consult with a podiatrist.
Cracked heels can be unpleasant to look at and may also cause a great deal of foot pain if left untreated. In serious cases, the cracks may turn into fissures, which are deep cracks in the skin that can lead to bleeding. While cracked heels are linked to dryness of the skin, they may also form due to a vitamin deficiency. If you aren’t getting the proper vitamin intake, the skin may become dry, dull, and prematurely age. Vitamin E is particularly beneficial in protecting collagen in your skin, and can be found in foods such as avocados, mangos, and salmon. For more information on what vitamins may help the prevention of cracked heels, please consult with a podiatrist.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact one of our podiatrists from Florida Foot & Ankle Group, P.A.. Our doctors can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact one of our offices located in Debary, Lake Mary, Orlando, and Oviedo, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels may make you want to think twice about showing off your feet in warmer weather. However, cracked heels may be harmful to more than just the appearance of your feet. If deep fissures and cracks develop in your heels, they may make walking and standing painful for you. Additionally, these openings make way for germs to enter through your skin and cause infection.
There are several different causes of cracked heels. One of the most common reasons for this ailment is dry skin. This problem may make your keeps feel rough tight and itchy. Dry skin may be caused by cold air, extremely hot water, harsh soaps, and aging. Skin disorders such as eczema and psoriasis may eventually lead to dry skin. In some cases, complications may arise from cracked heels. Some of these complications are a loss of feeling in the heel, cellulitis, or a diabetic foot ulcer.
There are ways you can try to prevent getting cracked heels. One of the best ways to do so is to avoid wearing flip flops and sandals because these shoes increase your risk of drying out your feet. You should also avoid wearing shoes with a tall skinny heel, because these shoes cause your heel to expand sideways. At night, you should slather on a thick moisturizing cream on your feet and then cover them in socks to keep your feet moisturized overnight. Drinking water to stay hydrated is also a good way to ensure that your skin doesn’t become dry.
If you suffer from a severe case of cracked feet, you should make an appointment with your podiatrist to see what treatment methods are best for you.
Increased BMI May Cause More Foot Pain
 Obesity can impact the health of your body in a variety of ways. But did you know that it can also impact the health of your feet? A recent study of over 2000 people found that overweight and obese people were more likely to experience foot pain. Furthermore, as BMI increased, so did the likelihood of experiencing foot pain. The explanation for this may be fairly simple. The feet support the weight of the entire body. As that weight increases, the feet are put under more pressure and strain, which can eventually lead to pain. If you experience foot pain, it is recommended that you see a podiatrist, who can provide a diagnosis and appropriate treatment options for you.
Obesity can impact the health of your body in a variety of ways. But did you know that it can also impact the health of your feet? A recent study of over 2000 people found that overweight and obese people were more likely to experience foot pain. Furthermore, as BMI increased, so did the likelihood of experiencing foot pain. The explanation for this may be fairly simple. The feet support the weight of the entire body. As that weight increases, the feet are put under more pressure and strain, which can eventually lead to pain. If you experience foot pain, it is recommended that you see a podiatrist, who can provide a diagnosis and appropriate treatment options for you.
The more you weigh, the harder your feet must work to support your body. If you’re an obese individual and are concerned about your feet, contact one of our podiatrists from Florida Foot & Ankle Group, P.A.. Our doctors can provide the care you need to keep you pain-free and on your feet.
Obesity and Your Feet
People who are overweight are putting more pressure on their ankles, knees, and hips as well as their feet. This unfortunately can lead to variety of different issues.
Problems & Complications Stemming from Obesity
- When the body is overweight, it tries to compensate by changing the way that it moves. An obese person may lean forward and put extra weight on the wrong part of the foot. This puts unnecessary stress on the feet.
- Obese people are also more likely to develop type II diabetes which is a condition that causes a lot of foot problems. People with diabetes often don’t feel the cuts and sores that they may have on their feet, which can lead to more complicated and severe issues.
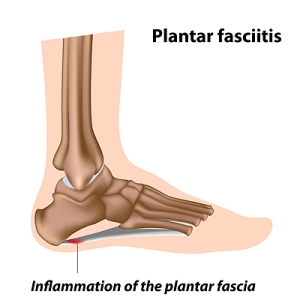
- Plantar fasciitis is another foot condition that can be caused by obesity. Plantar fasciitis is an inflammation of the tissue along the bottom of the foot, which causes pain and stiffness while walking and climbing stairs.
If you have any questions, please feel free to contact one of our offices located in Debary, Lake Mary, Orlando, and Oviedo, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Obesity and the Feet
Obesity is a common problem in American society. Approximately one third of the U.S. population is obese. Obesity is defined as a body mass index greater than 30. Obesity has the power to affect different aspects of the body, and one of the most common problems it causes is foot pain. There have been many studies that found a connection between an increased BMI and foot problems. A simple activity such as walking up a flight of stairs can increase pressure on the ankle by four to six times.
Being overweight causes the body to compensate for the extra weight by changing the way it moves. Consequently, people who struggle with obesity commonly have arch problems in their feet. Obesity causes the arch to break by stretching the ligaments and tendons that hold the bones in the foot together. When the arch lowers, the foot may eventually fall flat. Collapsed foot arches fail to provide adequate shock absorption which eventually leads to foot pain. Other conditions that may be caused by flat feet are pronation, plantar fasciitis, weak ankles, and shin splints.
Foot problems that are caused by obesity may be treated by wearing proper footwear. Proper shoes will allow your feet to have better circulation around the arch and ankle. Additionally, those with obesity often discover that typical heel pain remedies are not effective for them. They will find that their plantar fascia is easily injured, and it is often inflamed. The best way to treat this problem is to implement lifestyle changes. A few good ways to improve your diet are to reduce calories, fill up on fruits and veggies, and to limit sugars.
Custom foot orthotics can prevent foot problems if you’re carrying excess weight or are trying to lose weight. The purpose of orthotics is to provide shock absorption to decrease the amount of stress on the joints to prevent arthritis.
Treating Poor Circulation
 Poor circulation in the feet is a common condition with potentially serious consequences. Symptoms of poor circulation can include tingling, numbness, pain, a pins and needles sensation, and muscle cramps in the feet and ankles. If you experience poor circulation in your feet, it is strongly suggested that you seek the care of a podiatrist. A podiatrist can perform vascular testing to diagnose poor circulation. To manage your condition, the doctor may recommend lifestyle modifications, such as eating a balanced diet, doing light exercises, and quitting smoking. These changes can improve your circulation and reduce the risk of other cardiovascular complications, such as heart attack or stroke. The podiatrist may also prescribe medications or other treatments to increase blood flow to your legs and feet.
Poor circulation in the feet is a common condition with potentially serious consequences. Symptoms of poor circulation can include tingling, numbness, pain, a pins and needles sensation, and muscle cramps in the feet and ankles. If you experience poor circulation in your feet, it is strongly suggested that you seek the care of a podiatrist. A podiatrist can perform vascular testing to diagnose poor circulation. To manage your condition, the doctor may recommend lifestyle modifications, such as eating a balanced diet, doing light exercises, and quitting smoking. These changes can improve your circulation and reduce the risk of other cardiovascular complications, such as heart attack or stroke. The podiatrist may also prescribe medications or other treatments to increase blood flow to your legs and feet.
Poor circulation is a serious condition and needs immediate medical attention. If you have any concerns with poor circulation in your feet contact one of our podiatrists of Florida Foot & Ankle Group, P.A.. Our doctors will treat your foot and ankle needs.
Poor Circulation in the Feet
Poor blood circulation in the feet and legs is can be caused by peripheral artery disease (PAD), which is the result of a buildup of plaque in the arteries.
Plaque buildup or atherosclerosis results from excess calcium and cholesterol in the bloodstream. This can restrict the amount of blood which can flow through the arteries. Poor blood circulation in the feet and legs are sometimes caused by inflammation in the blood vessels, known as vasculitis.
Causes
Lack of oxygen and oxygen from poor blood circulation restricts muscle growth and development. It can also cause:
- Muscle pain, stiffness, or weakness
- Numbness or cramping in the legs
- Skin discoloration
- Slower nail & hair growth
- Erectile dysfunction
Those who have diabetes or smoke are at greatest risk for poor circulation, as are those who are over 50. If you have poor circulation in the feet and legs it may be caused by PAD and is important to make changes to your lifestyle in order to reduce risk of getting a heart attack or stroke. Exercise and maintaining a healthy lifestyle will dramatically improve conditions.
As always, see a podiatrist as he or she will assist in finding a regimen that suits you. A podiatrist can also prescribe you any needed medication.
If you have any questions please feel free to contact one of our offices located in Debary, Lake Mary, Orlando, and Oviedo, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes, Symptoms, and Treatment of Poor Blood Circulation in the Feet
Poor blood circulation in the feet and legs is often caused by peripheral artery disease (PAD), which is usually the result of a buildup of plaque in the arteries. Plaque buildup, or atherosclerosis, can be the result of excess calcium and cholesterol in the bloodstream. This restricts how much blood can flow through arteries. Reduced blood flow to a certain area of the body severely limits the amount of oxygen and nutrients that part of the body receives. This leads to degeneration in the muscles and other tissues. Sometimes, poor blood circulation in the feet and legs can be caused by other conditions, such as the damaging or inflammation of blood vessels, known as vasculitis.
The lack of oxygen and nutrients caused by poor blood circulation can restrict muscle growth and development, as well as cause muscle pain and cramps, weakness, and stiffness. Other common symptoms include numbness in the legs and feet, skin discoloration in the affected limbs, slower nail and hair growth, and erectile dysfunction in men. In more severe cases of PAD, pain can be present even when a person isn't exercising, and may range from mildly uncomfortable to completely debilitating.
Poor blood circulation in the feet and legs is more common in those who are overweight or obese, have diabetes, high blood pressure, high cholesterol, who smoke, or who have a family history of PAD or related conditions such as a heart attack, stroke, etc. Diabetes and smoking place a person at greatest risk for developing poor blood circulation, although advanced age, over 50, can also increase risk.
If you are experiencing poor blood circulation in the feet and legs caused by PAD, it is important to make changes to your lifestyle in order to reduce your risk of experiencing a heart attack or stroke caused by this condition. If you smoke, quit completely. This will increase the amount of oxygen in your bloodstream. Exercising and reducing the saturated fats in your diet. Saturated fats come from fatty meats, fried foods, whole milk, etc., can make a difference in improving blood circulation in feet. It is also important to avoid developing influenza and to carefully control your blood sugar if you have diabetes.
Your doctor may recommend combining lifestyle changes with a prescription medication regimen to improve blood circulation. The most commonly-used medications for PAD are called statins and work by blocking the amount of enzymes in your body that produce cholesterol. They are known by the brand names Zocor, Lipitor, Crestor, and others.
What Is Plantar Fasciitis?
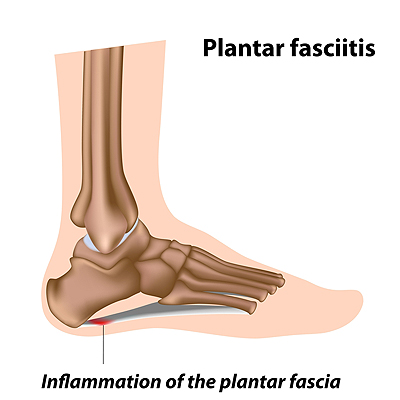 The plantar fascia is a thick band of fibrous tissue that connects the heel to the toes along the bottom of the foot. Since the plantar fascia works as a shock absorber and arch support, it can become painful when it is overloaded or overstressed. This pain is known as plantar fasciitis. Research has shown that pain is most commonly located on the inside of the heel and occurs during weight-bearing activities. A podiatrist will be able to examine the foot and heel for further issues, particularly a stress fracture. A podiatrist may also take X-rays or use an ultrasound machine to determine the extent of the injury. Some treatment options may include rest, a change in footwear, orthotics or physical therapy. If you believe that you may be afflicted with plantar fasciitis, it is important to check with a podiatrist for a proper diagnosis and treatment plan.
The plantar fascia is a thick band of fibrous tissue that connects the heel to the toes along the bottom of the foot. Since the plantar fascia works as a shock absorber and arch support, it can become painful when it is overloaded or overstressed. This pain is known as plantar fasciitis. Research has shown that pain is most commonly located on the inside of the heel and occurs during weight-bearing activities. A podiatrist will be able to examine the foot and heel for further issues, particularly a stress fracture. A podiatrist may also take X-rays or use an ultrasound machine to determine the extent of the injury. Some treatment options may include rest, a change in footwear, orthotics or physical therapy. If you believe that you may be afflicted with plantar fasciitis, it is important to check with a podiatrist for a proper diagnosis and treatment plan.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from Florida Foot & Ankle Group, P.A.. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact one of our offices located in Debary, Lake Mary, Orlando, and Oviedo, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.